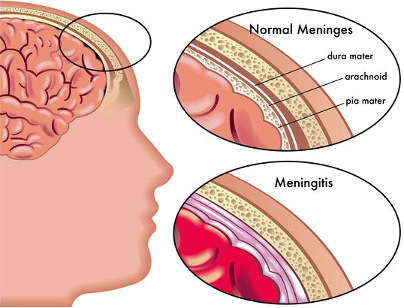
Meningitis means inflammation of the membranes ‘meninges’ lining the brain. Meningococcal is a bacteria that enters the body, however Meningococcal does not always lead to Meningitis. There are several forms of Meningitis, Meningococcal and Pneumococcal.
Government provided vaccinations are important and cover you for the most common strains, however they do NOT cover all strains. So, make sure you know the signs and symptoms
Some of the forms of Meningitis, Meningococcal and Pneumococcal include:
Bacterial meningitis is aggressive, develops quickly and can lead to permanent disability or death in a matter of hours if no medical attention is sought.
Most cases of bacterial meningitis are caused by:
- Meningococcus/meningococcal
- Pneumococcus/pneumococcal
- Haemophilus Infuenzae Type B/Hib
- Tuberculosis/TB
- Group B Streptococcus
- E.coli Meningitis
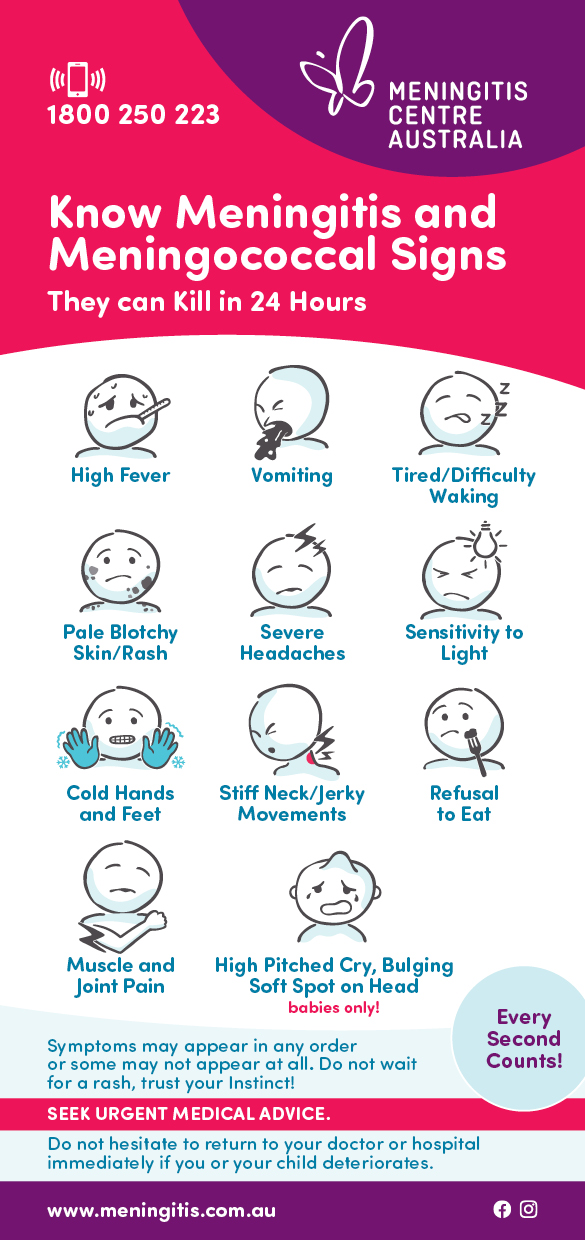
What are the Signs and Symptoms of bacterial meningitis?
The symptoms are usually flu-like with a runny nose, irritable, hates bright lights, fever, and maybe seizures. Visit our signs and symptoms page for the full list.
Please do NOT wait for a rash to appear before seeking medical attention!
What is the treatment for bacterial meningitis?
Bacterial meningitis is life threatening and needs urgent medical attention. To diagnose properly what strain or type of bacterial meningitis, the patient requires an invasive procedure called a lumbar puncture which is a needle inserted into the base of the spine to test the spinal fluid for the bacteria. Once or if the strain is determined, the patient is then given antibiotics to aid their recovery.
How and why do you get meningitis?
Bacterial meningitis can affect anyone, anywhere and at any time. It is not seasonal, age or cultural bias. Infants in particular are more prone to contracting bacterial meningitis because their immune system is so immature.
Teenagers and young adults are known to be the biggest carriers of the disease because they socialise in close knit groups, attend festivals and mosh pits, parties, have late nights and share, food, cigarettes, drinks and engage in intimate kissing where transmission of the bacteria is more likely.
Australia has 5 common strains of meningococcal disease they are: Men A, Men B, Men C, Men W-135 and Y. They are all preventable through vaccination.
Meningococcal B is the most common strain in Australia however Meningococcal W-135 follows a close second, is more aggressive and has a higher mortality rate than most of the other strains.
It’s believed 30% of the population carries the bacteria in the back of our nose and throat without being aware of it.
On rare occasions the bacteria can defeat the body’s immune system and cause infection. This might be due to the person feeling rundown, late nights, stress, or illness.
Most often the bacteria are spread through sneezing, coughing or being more intimate, like deep kissing.
When the bacteria travels through the bloodstream and affects the meninges (the lining between the skull and brain which is filled with cerebrospinal fluid) it becomes meningitis or a purple rash may develop causing septicaemia
Australia is very progressive with its vaccines and has the ACWY vaccination on its National Immunisation Program. Several states offer other types of vaccinations for meningococcal disease.
Meningococcal meningitis, caused by Neisseria meningitidis bacteria, is of particular importance due to its potential to cause large epidemics. There are twelve strains, which have been identified, seven of which (A, B, C, E, W-135, X and Y) can cause epidemics.
The largest burden of meningococcal disease occurs in an area of sub-Saharan Africa known as the meningitis belt, which stretches from Senegal in the west to Ethiopia in the east (26 countries). During the dry season between December to June, dust winds, cold nights and upper respiratory tract infections combine to damage the nose and throat area, increasing the risk of meningococcal disease. At the same time, transmission of the bacteria can be accelerated due to overcrowding of housing. This combination of factors explains the large epidemics which occur during the dry season in the meningitis belt. Meningococcal strains A, C, W-135 and X are most common here.
Meningococcal Septicaemia
Meningococcal septicaemia is when the meningococcal bacteria multiplies in the blood and releases poison that damages the body.
The toxins stop the important flow of oxygen to the organs including the skin and the surrounding tissues causing purple spots which can develop into something that looks like a rash. This is also known as blood poisoning and URGENT medical attention is needed as the person is in a critical condition.
After Effects of Meningococcal Septicaemia
The damage that the toxins cause in the bloodstream and eventually to the organs and limbs can result in the following:
- Skin and tissue damage
- Skin grafts
- Bone growth problems
- Organ failure
- Limb loss
- Prosthetics for the patient
Pneumococcal meningitis is a rare but very serious illness that can develop into a life-threatening medical emergency. The infection may have long-term consequences and can even be fatal. Prompt treatment is necessary to minimize the risk of adverse outcomes.
Streptococcus pneumoniae (S. pneumoniae) is a widespread bacterium responsible for many illnesses, including meningitis, pneumonia and sinus infections. The bacteria are spread easily and quickly from person to person through coughing and sneezing.
S. pneumoniae is the most common cause of bacterial meningitis in adults and in children under 2 years old.
There are over 90 different strains but only a small amount cause the disease. It usually sits harmlessly in the back of the throat by both adults and children.
It is usually released in the air through sneezing, coughing, intimate kissing. Most of the bacteria are transferred to the meninges through the bloodstream and infects the cerebrospinal fluid (CFS).
The incidence of severe pneumococcal infection, including meningitis, has decreased significantly since the introduction of the pneumococcal vaccine on to the Australian National Immunisation Plan in 2005 which is given to babies, at risk groups and seniors.
Risk Factors
Certain factors can make a person more susceptible to developing pneumococcal meningitis, including:
- decreased immune response from infection or drug use
- diabetes
- trauma or injury to the head
- recent ear infection with pneumoniae
- history of meningitis
- alcohol consumption
- cigarette smoking
- removed or non-functioning spleen
- chronic liver, lung, renal, or heart disease.
- infection of a heart valve with pneumoniae
- having a cochlear implant
- recent case of pneumonia with pneumoniae
- recent upper respiratory infection
After Effects
- Pneumococcal meningitis can leave people with serious after effects including:
- Loss of hearing
- Epilepsy
- Brain injury
- Severe mental retardation
- Memory loss
- Inability to talk
- Inability to walk
Viral meningitis is the most common but the least severe type. Almost all patients recover without any permanent damage, although full recovery can take many weeks.
It is most often spread through respiratory droplets (kissing, coughing, sneezing) or faecal contamination. Elderly people and those with conditions that affect their immune system are more at risk.
Most cases of viral meningitis are caused by enteroviruses (common stomach viruses). However, other viruses can also cause viral meningitis. For instance, West Nile virus, mumps, measles, herpes simplex types I and II, varicella, and lymphocytic choriomeningitis (LCM) virus.
Viral meningitis cannot be reliably differentiated from bacterial meningitis, however viral meningitis has no evidence of bacteria present in the cerebrospinal fluid. A lumbar puncture is often needed to identify the disease.
The symptoms are usually the inflammation of the meninges (the membrane covering the brain and spinal cord). Symptoms commonly include headache, fever, sensitivity to light and neck stiffness.
There are no vaccines available for viral meningitis, but washing hands thoroughly and keeping surfaces clean can help prevent the disease.
Group B Streptococcus is bacteria that live harmlessly in the intestinal tract or the vagina.
It is believed around 10%-30% of pregnant women carry the GBS bacteria; however the majority of the babies will not become ill with the disease.
Newborn babies who contract GBS become infected because their immune system is underdeveloped. The bacteria can spread through the blood and cause serious illness like meningitis, septicaemia or pneumonia.
Risk of GBS in babies
- The mother had a previous baby with GBS
- Urine and swab tests positive for GBS in the mother
- Mother has a high temperature during labour
- Baby is part of a multiple birth
- Premature baby
- Labour is longer than 18 hours after waters have broken.
Late onset of the disease
Late-onset GBS infection is associated with the mother carrying GBS or being very young (under 20 years) and the baby being born preterm (before 37 weeks of pregnancy)
Some babies may contract GBS between 7 and 28 days after birth and is usually contracted when babies come in contact with someone whose hands may contain the GBS bacteria.
Symptoms of GBS in babies
- Fever (could have cold hands and feet)
- Not being able to feed
- Vomiting or diarrhoea
- Dislikes being handled
- Difficulty breathing/grunting
- Pale/blotchy skin
- High pitched cry or moaning
- Bulging soft spot on head (fontanelle)
- Arched back
- Swollen abdomen
- Dry nappy/diaper
- Blotchy pale skin
- Red or purple spots – DO NOT WAIT FOR THE RASH TO OCCUR
Treatment for GBS
Babies with suspected GBS disease need to seek urgent medical attention. Ask the nurse or the doctor could it be meningitis or GBS?
Prevention of GBS
- There is no vaccine to protect against GBS.
- Those women who are at a higher risk of GBS can be given antibiotics to reduce the risk during labour and can also be given to babies immediately after birth.
- You can be tested for GBS in late pregnancy. Speak to your GP about the ECM (Enriched Culture Medium) test.
This is a rare form of meningitis in Australia. It usually develops slowly. Most people contract this disease through poor living standards and through other illnesses like HIV infection. TB meningitis is common in children under 5 years of age because of their low immunity.
Those who suffer from TB which usually affects the lungs can progress to TB meningitis, but it is rare.
Because the disease progresses slowly it is often difficult to diagnose and it is often advanced before treatment begins.
Like most meningitis, the bacterium enters the body through droplet inhalation – sneezing or coughing from an infected person.
If the bacteria travel through to the brain or the meninges, small abscesses form. These abscesses can burst and cause TB meningitis.
The infection causes pressure on the brain resulting in nerve damage.
Countries where TB is prevalent
- Africa
- South East Asia
- East Mediterranean
- Western Pacific
- Russia
- China
- South America
Treatment for TB meningitis
Once the patient is diagnosed with TB meningitis a series of antibiotics are administered including steroids. An individual care plan will be arranged with your doctor.
You can also get vaccinated against TB through the BCG vaccination and this is recommended for those people who travel to the above countries on a regular basis like Fly-in-Fly-Out (FIFO) workers.
Neonatal meningitis occurs in the first two months of life and can be caused by a variety of different organisms including Streptococcal B, E.coli and Listeria.
It is a rare disease, but if not treated immediately babies can die or be left with serious after effects including, disability or limb loss.
A lumbar puncture is usually needed to determine whether the infant has the disease.
Symptoms
- Fever (could have cold hands and feet)
- Not being able to feed
- Vomiting or diarrhoea
- Dislikes being handled
- Difficulty breathing/grunting
- Pale/blotchy skin
- High pitched cry or moaning
- Bulging soft spot on head (fontanelle)
- Arched back
- Swollen abdomen
- Dry nappy/diaper
- Blotchy pale skin
- Red or purple spots – DO NOT WAIT FOR THE RASH TO OCCUR
Haemophilus influenzae type b (Hib) disease is a serious disease caused by bacteria. It is a type of bacteria, which can cause many different kinds of infections. These infections range from mild ear infections to severe diseases, like bloodstream infections. It usually affects children under 5 years old. It can also affect adults with certain medical conditions and may start off as Bronchitis.
You can get Hib disease by being around other children or adults who may have the bacteria and not know it. The germs spread from person to person. If the germs stay in the child’s nose and throat, the child probably will not get sick. But sometimes the germs spread into the lungs or the bloodstream, and then Hib can cause serious problems. This is called invasive Hib disease.
Side Effects from Hib
- Brain damage
- Hearing loss
- Pneumonia
- Severe swelling in the throat, making it hard to breathe
- Infections of the blood, joints, bones, and covering of the heart
- Death
Australia introduced a vaccine for Hib on to its National Immunisation Plan in 1993 and babies from the age of 2 months are now vaccinated against the disease.
Amoebic meningitis is an infection of the brain and its lining known as the meninges. It is a very rare form of meningitis and usually occurs when a person has ingested water which is dirty and unfiltered.
The amoeba that causes the infection occurs in shallow surface waters and badly maintained swimming pool, spas, still river beds and lakes and is usually seen in warmer climates.
Infection occurs when infected water enters the nose. This can happen when diving, jumping or swimming in fresh water. The amoeba then invades the brain and meninges through the nose. This is a rare disease affecting mainly young active people. It is almost always fatal.
E.coli meningitis is the second most common bacterial cause of neonatal meningitis second to Streptococcus B.
Women carry the bacteria in their intestines and vagina and babies who develop neonatal meningitis can develop the infection when exposed to the bacteria during delivery.
Premature and low birth-weight babies are at much higher risk. It is a very serious disease. Approximately 20% of newborns die in spite of treatment, and many survivors sustain permanent brain damage. Because most cases occur in premature infants it is difficult to determine how much of the damage is due to meningitis and how much is the result of premature birth.
E.coli meningitis is treated with antibiotics and in spite of much research no vaccine has yet been developed.
Mollaret’s meningitis is named after the person who discovered it in 1944, Pierre Mollaret (pronounced as Molla-ray). It is a rare type of chronic recurrent, lymphocytic meningitis often caused with the Herpes Simplex virus type 2.
Herpes Simplex virus type 2, directly affects the central nervous system and can be inactive for a time without the person showing any signs or symptoms.
About 1 in 5 people who suffer from the Herpes Simplex Virus 2 meningitis more than three times is usually diagnosed with Mollaret’s meningitis.
Mollaret’s can last between 2-7 days and usually resolves itself, however there is medication for this and is usually similar to the medicine used to treat genital herpes and cold sores. It is necessary to see your doctor for advice and perhaps a neurological infection specialist.
For further information on this go to https://mollaretsmeningitis.org/
Fungal meningitis is rare, however the most common cause is Cryptococcus spp. infection, but many other fungi may occasionally cause meningitis.
Fungal meningitis is not transmitted from person to person. The fungi are usually inhaled and then spread by the blood to the central nervous system; fungi may also be directly inserted into the central nervous system by medical techniques or enter from an infected site near the central nervous system to cause meningitis.
Fungal meningitis is rare and usually the result of spread of a fungus through blood to the spinal cord. Although anyone can get fungal meningitis, people with weakened immune systems, like those with HIV infection or cancer, are at higher risk.
The most common cause of fungal meningitis for people with weakened immune systems is Cryptococcus. This disease is one of the most common causes of adult meningitis in Africa.
You may also get fungal meningitis after taking medications that weaken your immune system. Examples of these medications include steroids (such as prednisone), medications given after organ transplantation, or anti-TNF medications, which are sometimes given for treatment of rheumatoid arthritis or other autoimmune conditions.
Different types of fungus are transmitted in several ways. Cryptococcus is thought to be acquired through inhaling soil contaminated with bird droppings, and Histoplasma is found in environments with heavy contamination of bird or bat droppings. Blastomyces is thought to exist in soil rich in decaying organic matter. Coccidioides is found in the soil of endemic areas. When these environments are disturbed, the fungal spores can be inhaled. Meningitis results from the fungal infection spreading to the spinal cord. Candida is usually acquired in a hospital setting.
Treatment
Fungal meningitis is treated with long courses of high dose antifungal medications, usually given through an IV line in the hospital. The length of treatment depends on the status of the immune system and the type of fungus that caused the infection. For people with immune systems that do not function well because of other conditions, like AIDS, diabetes or cancer treatment is often longer.
Prevention
No specific activities are known to cause fungal meningitis. Avoid soil and other environments that are likely to contain fungus. People with weakened immune systems (for example, those with HIV infection) should try to avoid bird droppings and avoid digging and dusty activities, particularly if they live in a geographic region where fungi like Histoplasma, Coccidioides, or Blastomyces species exist. HIV-infected people cannot completely avoid exposure.
More information
If you would like more information on this you can download our brochures and pamphlets, find out more about vaccines, call us Monday-Friday on 1800 250 223 or email us at info@meningitis.org.au