We had gone to the city for a long weekend and on our second night Nathaniel developed a very high temperature. We treated it with pain relief medication and during the day he was fine. His temperature returned at night and he was also breathing rapidly but again Panadol controlled it.
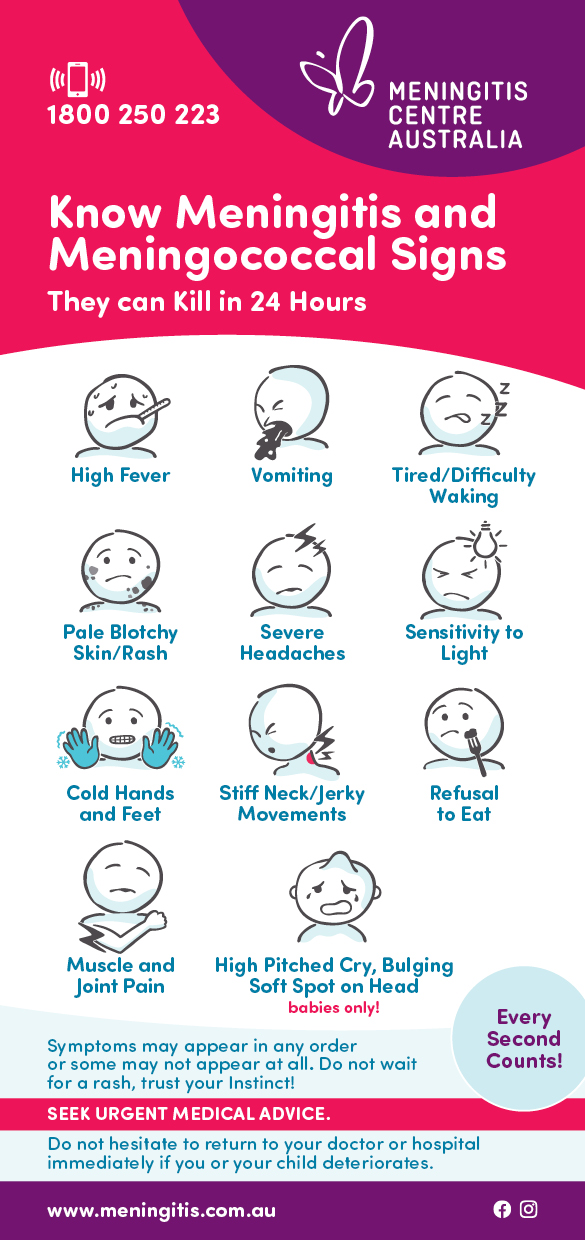
He seemed fine, if a little more tired than usual, for the long drive home. Once we got home Nathaniel ate a big dinner and went to bed. He slept in his own bed the entire night (which was unusual for him) and even ‘slept in’. In the morning he came into our bedroom and said his head hurt. I rang the doctor immediately and she saw us first thing. The doctor examined Nathaniel and checked for neck stiffness, light sensitivity and rashes and none were present. She told me to alternate two different pain relief medications for the day, to keep and eye on Nathaniel and come back if he got any worse or if I was worried.
I put Nathaniel on the couch in the lounge where I could watch him easily. He vomited soon after we got home. However I did not think it was anything too sinister, as my children often vomited when they had a temperature and it was obvious he had just brought up his milk. He slept most of the day and I would rouse him for a drink every 30 minutes and ask if he was all right. Nathaniel could barely keep his eyes open but he would always respond when I spoke to him and say ‘Mummy’ or ‘Alright Mummy’.
By mid afternoon he hadn’t moved position on the couch and I was worried he might be uncomfortable, so I tried to move him. He did not want to move and his body seemed to be stiff and in pain so I got him some more Panadol. He was still saying he was all right. He then went back to sleep. Later that afternoon he seemed to be worse so I rang my husband then my Mum and asked my Mum to come and look at Nathaniel. She also agreed that he looked worse and by that stage he had vomited up green stuff. We rang the doctor again who told us to call an ambulance and get Nathaniel straight to hospital.
We live two minutes from the hospital so Mum drove us there. He was still saying ‘Mummy” in the car but by the time we got him into the hospital he was semi-conscious and completely unresponsive. When we arrived at the hospital, it was like a scene from ‘ER’ with doctors and nurses surrounding Nathaniel, poking and prodding him. It seemed like every single doctor and nurse wanted to know the whole story of Nathaniel’s illness. They started asking questions about seizures and cold sores. During this time Nathaniel was staring blankly to one side, unable to move his eyes or his head and completely unresponsive. As long as I live I will not forget the look on his face. He did not even flinch when they put needles into his arm.
We saw the emergency department doctor who advised us that Nathaniel might have meningitis. The medical staff had already taken blood and began giving Nathaniel several different intravenous antibiotics. The paediatrician came and confirmed the diagnosis. We were told that Nathaniel would need to be flown to one of the major city children’s hospitals (which might be interstate) so he could be admitted to a specialist Paediatric Intensive Care Unit (PICU).
In the end we were flown to a strange interstate city where we knew no one and we thought we might not bring Nathaniel home again. Before the retrieval team arrived to transport Nathaniel to the interstate hospital he started to have breathing problems. An anaesthetist was called to intubate Nathaniel (that was the worst thing I have ever watched). We were told that this would have been needed anyway for the plane trip. When the ‘retrieval team’ arrived they seemed to spend hours getting Nathaniel ready. The journey to the interstate city hospital took about an hour and we arrived in the early hours of the morning. Nathaniel was settled into the PICU. I sat with him for a while, and then was sent to bed in a nearby room, with a promise from the nurses, that they would call me if anything happened. I emerged from my rest about four hours later to find Nathaniel in the same state that I left him. I finally plucked up the courage to ask if Nathaniel was going to die. I was hoping they would say, “No, of course not, he will be fine.” However I was told the survival statistics for meningitis patients, that Nathaniel was in the best place and they were doing everything that they possibly could.
A couple of hours later the preliminary blood test results were phoned through from the local hospital where Nathaniel was first seen. The doctors were pretty sure it was Pneumococcal Meningitis. A short time later the preliminary diagnosis was confirmed. Later that afternoon I received a phone call from my husband who told me that Nathaniel’s twin had been admitted to our local hospital and tested for meningitis. Nathaniel’s brother had developed a very high temperature so the doctors also gave him intravenous antibiotics while they waited for the results of his blood tests. It turned out he just had a throat infection. Consequently my husband was unable to get to the interstate city hospital because Nathaniel’s twin brother was also admitted to our local/regional hospital. I was terrified Nathaniel might die and my husband would be unable to say goodbye. Thankfully that did not happen.
On the second day in the city hospital the doctors were confident that Nathaniel was improving and they decided to extubate him. I felt confident to leave him and go and have a shower. Before I left I whispered in his ear that I would be back in five minutes and that I was going to wash my hair. I knew he was all right when I returned to the PICU and I heard him saying “No hair wash mummy”. From that moment on, Nathaniel seemed to get better. Later that day we were moved out of the PICU and onto a busy ward. A day later we were told Nathaniel could be transferred back to our local hospital. My husband organised a return flight to our local hospital where Nathaniel and I spent another four days. Nathaniel spent a total of ten days in hospital.
When we went home I thought everything would be okay. Nathaniel passed his hearing test and only required one physiotherapy appointment. The medical staff told us that the only follow up we would require would involve regular appointments with the paediatrician, until Nathaniel started school. This was needed to monitor his recovery and identify any possible developmental problems. Unfortunately we have recently noticed problems with Nathaniel’s vision. Nathaniel has developed Nystagmus (involuntary eye movements) as well as a squint and we have had to start a new round of specialist visits and tests. The tests have ruled out some serious conditions such as tumours, epilepsy and serious brain damage but have also been inconclusive, so we have to return to the city hospital for further tests in the coming weeks. Although we are unsure what is the cause the visual problems, we feel extremely lucky and grateful to have a reasonably healthy child at the end of this horrendous ordeal.
Our experiences with medical personnel were okay. However we would have liked hospital medical staff to have spent more time explaining what was happening, as both my husband and I were so shocked when we were told Nathaniel had pneumococcal meningitis. Our GP was devastated when she discovered how sick Nathaniel had been. We remain extremely thankful to all the doctors and nurses who looked after Nathaniel in the emergency room. Both the emergency doctor and nurse who saw Nathaniel had seen meningitis before and knew exactly what to do. We were told more than once in the city hospital that the local hospital staff had probably saved Nathaniel’s life.
To look at Nathaniel now you would not know how sick he had been. However his personality has changed a little. He is often scared to go to bed and he is more clingy and wary of strangers (particularly if they are wearing colours that are used in nurse’s uniforms). Nathaniel is very frightened of the doctor, which was not the case before he became ill with meningitis. He also gets quite distressed when he sees a photograph of himself in hospital. He is a little clumsier than he used to be and also gets the odd headache. His vision problems seem to be the only ongoing issue.
I do not think any amount of prior knowledge of this disease could have helped us. I thought I knew the symptoms of meningitis but Nathaniel really did not exhibit typical symptoms until he was already gravely ill. At our first post hospital appointment with the paediatrician he said, “Well, now you know what meningitis looks like, so if it ever happens to you again, you will know.” However I don’t think I would. We have become more cautious about the children’s health than we were before Nathaniel became ill and we visit the doctor more. The other thing that keeps going through our mind is that we were not aware of how serious pneumococcal disease can be.
We live in an area with a large Aboriginal population so there are many advertising campaigns, such as “No more Pneumococcal” ads on TV and numerous brochures at the Health Centre and at the doctor’s practice. However these seem to talk about the more common pneumonia. The pneumococcal vaccine was as far as we were aware, only available to Aboriginal people and other groups who are at increased risk of catching pneumococcal disease. Nobody ever told us that healthy children could get this disease!!! We had heard about the meningococcal bacteria and we had the children vaccinated with the meningococcal C vaccine. However we did not realise that there were other types of bacteria that could cause meningitis and that we could still get this disease.